Transcranial Magnetic Stimulation (TMS) therapy has emerged as an innovative treatment option for individuals suffering from major depressive disorder (MDD) and other mental health conditions that have not responded well to traditional treatments. Many people considering this therapy wonder, does United Health Community Plan cover TMS treatment in Texas? Understanding insurance coverage for mental health treatments can be complex, but it is crucial to ensure access to necessary care. This article explores TMS therapy, UnitedHealthcare’s coverage policies, and how individuals can navigate their insurance plans to access this transformative treatment.
Understanding TMS Therapy
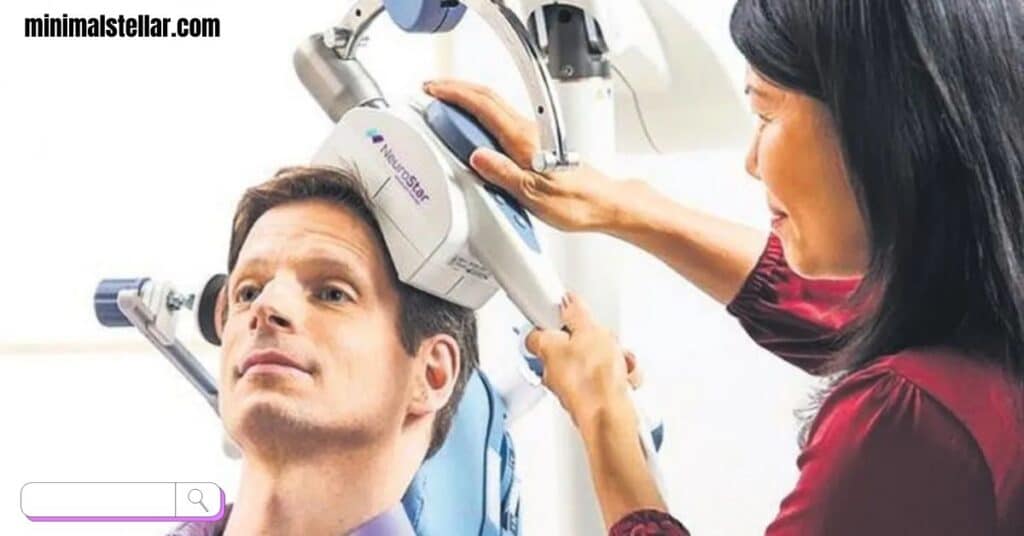
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. It is primarily used to treat depression, particularly in individuals who have not found relief through medication or psychotherapy. During a TMS session, an electromagnetic coil is placed against the patient’s scalp, delivering repetitive magnetic pulses to targeted areas of the brain associated with mood regulation.
Unlike traditional antidepressant medications, TMS does not cause systemic side effects such as weight gain, sexual dysfunction, or drowsiness. This makes it an appealing option for patients seeking an alternative or complementary treatment for their mental health conditions. TMS therapy has been approved by the Food and Drug Administration (FDA) for treating major depressive disorder, obsessive-compulsive disorder (OCD), and certain neurological conditions. Ongoing research suggests that it may also be beneficial for treating anxiety, post-traumatic stress disorder (PTSD), and bipolar disorder.
The therapy is typically administered over several weeks, with patients receiving multiple sessions per week. Each session lasts between 20 and 40 minutes. Since the treatment does not require anesthesia or sedation, patients can resume their daily activities immediately afterward. Many individuals report significant improvements in their mood and overall well-being after completing the treatment regimen.
UnitedHealthcare Coverage for TMS Therapy
UnitedHealthcare (UHC) provides health insurance coverage for millions of Americans through various plans, including employer-sponsored insurance, individual health plans, and government-funded programs like Medicare and Medicaid. Whether UHC covers TMS therapy depends on several factors, including the specific plan, medical necessity, and policy guidelines.
Eligibility Criteria for TMS Coverage
UnitedHealthcare covers TMS therapy under certain conditions. To qualify for coverage, patients typically need to meet the following criteria:
- Must be at least 18 years old
- Must have a diagnosis of major depressive disorder (MDD)
- Must have tried and failed at least two different antidepressant medications
- Must have undergone psychotherapy without significant improvement
- Must not have medical contraindications for TMS therapy
These requirements are designed to ensure that TMS therapy is provided to individuals who truly need it. In the past, UnitedHealthcare required patients to try at least four different antidepressants before approving TMS treatment. However, recent policy updates have made the process more accessible by reducing the number of failed medication trials to two and eliminating the mandatory psychotherapy requirement.
Does United Health Community Plan Cover TMS Treatment in Texas?
United Health Community Plan is a Medicaid-managed care plan offered by UnitedHealthcare in various states, including Texas. The plan provides healthcare coverage for low-income individuals and families, offering access to essential medical services, preventive care, and specialized treatments.
When it comes to TMS therapy, coverage under United Health Community Plan varies based on state regulations and medical necessity. In Texas, Medicaid programs, including United Health Community Plan, typically follow strict guidelines for covering mental health treatments. While TMS therapy may not be universally covered under all Medicaid plans, some patients may qualify if they meet the necessary criteria and receive prior authorization from their healthcare provider.
To determine eligibility for TMS therapy under the United Health Community Plan in Texas, patients should:
- Consult with their primary care physician or psychiatrist to assess whether TMS therapy is a suitable treatment option.
- Obtain a formal diagnosis of major depressive disorder or another qualifying condition.
- Provide documentation of previous treatment attempts, including medication trials and psychotherapy sessions.
- Work with their healthcare provider to submit a prior authorization request to UnitedHealthcare.
Since Medicaid policies vary, individuals should contact UnitedHealthcare directly or review their plan documents to confirm coverage details for TMS therapy in Texas.
How American TMS Clinics Can Help Patients Access Treatment

Navigating insurance coverage for TMS therapy can be overwhelming, but specialized treatment centers like American TMS Clinics are equipp to assist patients in understanding their benefits and securing approval for treatment. These clinics have experience working with insurance providers, including UnitedHealthcare, and can help streamline the verification and approval process.
Personalized Insurance Assistance
At American TMS Clinics, insurance specialists work closely with patients to determine their eligibility for TMS therapy. They guide individuals through the pre-authorization process, ensuring that all require documentation is submitt correctly. By handling the administrative aspects of insurance coverage, the clinic allows patients to focus on their treatment and recovery without unnecessary stress.
Comprehensive Mental Health Care
Beyond insurance assistance, American TMS Clinics provide comprehensive mental health services tailored to each patient’s needs. From initial consultations and treatment planning to post-therapy support, these clinics are committe to helping individuals achieve lasting improvements in their mental well-being. The combination of cutting-edge TMS technology and compassionate care ensures that patients receive the highest quality treatment available.
The Hidden Truth About Sono Bello Nightmares: What You Need to Know
Taking the Next Steps
For individuals considering TMS therapy as a treatment for depression or other mental health conditions, understanding insurance coverage is a crucial step. If you are wondering, does United Health Community Plan cover TMS treatment in Texas?, the best approach is to contact UnitedHealthcare directly and consult with a qualified TMS provider.
American TMS Clinics can provide guidance on insurance verification, eligibility requirements, and treatment options, ensuring that patients receive the care they need. By taking proactive steps and seeking expert assistance, individuals can navigate the insurance process with confidence and access the mental health treatment they deserve.
How to Choose the Perfect Fashion Nails for Your Style
Frequently Asked Questions (FAQs)
How to Choose the Perfect Fashion Nails for Your Style
Yes, UnitedHealthcare covers TMS therapy for eligible patients who meet the necessary medical criteria, including a diagnosis of major depressive disorder and prior unsuccessful treatment attempts.
How can I find out if my UnitedHealthcare plan covers TMS therapy?
You can check your insurance benefits by contacting UnitedHealthcare directly, reviewing your policy documents, or consulting with a TMS treatment provider who can assist with insurance verification.
Is TMS therapy cover by Medicaid in Texas?
Coverage for TMS therapy under Medicaid, including United Health Community Plan in Texas, depends on medical necessity and prior authorization. Patients should check with their insurance provider for specific details.
How long does it take to get approve for TMS therapy?
The approval process varies depending on the insurance provider and individual case. It typically takes a few weeks to obtain authorization once all necessary documentation is submitted.
What should I do if my insurance denies coverage for TMS therapy?
If your insurance denies coverage, you can appeal the decision by providing additional medical documentation, seeking assistance from your TMS provider, or exploring alternative financing options for treatment.
By understanding the coverage policies and taking proactive steps, patients can improve their chances of receiving TMS therapy and finding relief from their mental health conditions.

Eliana Amelia is the insightful author behind Minimal Stellar. With extensive experience in blogging, she expertly crafts content on the latest hair trends and cutting techniques. Eliana’s passion for haircare and style, combined with her professional expertise, ensures that her readers receive valuable, up-to-date advice. Her dedication to helping others look and feel their best shines through in every post.







